The Haitian Population Speaks Creole
Learning in a mother language (first language) is incredibly important to children’s further development and education. Early grade reading instruction should be in a language children speak and understand. When the instruction is in an unfamiliar language, an enormous amount of time must be spent first teaching children to understand, speak, read, and write that foreign language. This is difficult in low resource contexts and wastes valuable time in the early grades. (USAID 2013)
Learning in a familiar language improves school outcomes, reduces repetition and reduces dropout. Children with instruction in their mother tongue are significantly more likely to be enrolled and attending school. Children learn to read faster if they speak the language of instruction because they already have the vocabulary, knowledge of the construction of the language, and the ability to pronounce the sounds of the language. This knowledge facilitates children’s learning to read and understand what they read. (USAID 2013)
The challenging socioeconomic circumstances surrounding the state of Haitian education are furthermore aggravated by the historical retention of the colonial French language spoken fluently by an estimated 5% of the Haitian population. The French language is the official language of the education sector, all the didactic material and the related testing for graduation is in French. The Haitian population speaks Creole. (“Didactic” Greek didaktikos, from didaskein “to teach”)
Starting in early 2000′s under the policies of president Jean-Bertrand Aristide Creole became the official language of government. Under President Aristide, the Ministry of Education has promoted Creole as a language and an ongoing trend of learning in the native Creole language. Most classrooms in Haiti operate in Creole with none or low comprehension of the textbooks still written in French.
Teachers’ inability to access professional development at “Ecole Normale”, limited income, and the French language as the official language of education, are the primary reasons why most teachers are under qualified.
When teachers engage their students in quality literacy circle in a culturally relevant environment it allows the student the opportunity to interpret from more than one perspective and point of view; be purposeful and reflective; and promotes curiosity, inquiry, and critical thinking.
Haiti Now directly purchases and distributes school books needed by the students. The Book Bank program is ongoing. This program provides school books to students for all subjects and facilitates professional development to their teachers. All textbooks will be retrieved and redistributed to new students each school year.
The objective is to increase academic achievements, improve the teaching and learning opportunity and the overall quality of education. The Book Bank program empowers marginalized children of poverty and Restavek with school books and their teachers with didactic material, pedagogy training, continuing education and assessments of literacy.

All children should have a medical history (if known) and physical examination.
Components of the medical history should include:
- History of trauma
- Symptoms of communicable disease (i.e. fever, coryza, cough, rash, diarrhea, vomiting)
- Past medical and surgical history including any known chronic diseases
- Specific history of TB and HIV should be solicited
- Medication history
Components of the physical examination should include:
- Vital signs and assessment of hydration status
- Height, weight, head circumference (if age appropriate)
- Obvious injuries that may have resulted from trauma
- A full physical examination with particular attention paid to signs that may indicate underlying medical problems such as heart disease, asthma, chronic malaria (e.g. tachycardia, heart murmurs, labored respiration, abdominal tenderness) or undetected but subtle injury from trauma (e.g. splenic rupture).
- Assessment of nutritional status (looking for signs of malnutrition)
If fever is present, there should be a high clinical suspicion of malaria, dengue fever, and typhoid. Consideration should also be given to detecting clinical conditions requiring isolation (i.e. typhoid, TB, measles or chickenpox). Optimally, evaluation should be performed in consultation with an expert in infectious diseases or tropical medicine.
Orphans with known chronic medical conditions (e.g. asthma, congenital cardiac conditions, seizure disorders) should be carefully evaluated and treated, particularly since previous therapy may have been disrupted. Orphans with known chronic cardiac and respiratory disease should have vital signs assessed including oxygen saturation (portable oximeter) as soon as possible. Orphans with diabetes should have a glucose measurement as soon as possible. Further, in 2009, the Haitian National Nutrition Survey found an acute and chronic malnutrition to be 4.5% and 24-35%, respectively.
Laboratory screening tests should include:
- Complete blood cell count with red blood cell indices
- HIV testing
- Malaria smear (if symptomatic)
- Stool examination for ova and parasites (3 specimens)
- Stool examination for Giardia spp., Cryptosporidium, rotavirus antigen (if symptomatic); Strongyloides serology if eosinophilia
- Syphilis serologic testing
- Non-treponemal test (RPR, VDRL, ART)
- Treponemal test (MHA-TP, FTA-ABS)
- Serologic testing for vaccine preventable diseases (if indicated—see text)
- Tuberculin skin test or Chest radiograph (see text)
Tuberculosis
The incidence of TB in Haiti is one of the highest in the Western hemisphere, at 306/100,000 for all forms of TB.
By comparison, the US rate is 4.2 per 100,000 (source: Global Tuberculosis Control: epidemiology, strategy, financing: WHO report 2009.
If adequate follow up can be guaranteed, screening orphans 2-14 years of age with the tuberculin skin test(TST) or interferon-gamma release assay (IGRA) is recommended. Physicians should be advised that some experts prefer TST in children younger than 5 years of age. There are relatively few published reports documenting the performance of IGRAs in young children, obtaining sufficient blood is more difficult, and there is concern that IGRAs may perform differently in very young children who are at greater risk of a poor outcome if an infection is undiagnosed. If the TST is ≥10 mm or IGRA is positive, a chest radiograph (CXR) (anteroposterior or posteroanterior view and a lateral view for applicants <10 years of age; a posteroanterior view for applicants >10 years of age) should be performed. If adequate follow-up cannot be guaranteed, the TST or IGRA can be omitted and a CXR can be done as the initial screening test. The following categories of children should provide sputum specimens:
- Orphans with signs and symptoms of TB
- Medical history suggesting TB
- CXR findings suspicious of TB
- HIV infection
Three sputum specimens (or alternative specimens such as gastric aspirates if the child cannot provide sputum specimens) should be provided to undergo microscopy for acid-fast bacilli (AFB), as well as culture for mycobacteria and confirmation of the Mycobacterium species, at least to the M. tuberculosis complex level. Orphans diagnosed with TB disease should be started on treatment with treatment delivered as directly observed therapy (DOT). Once the orphans are in a long-term placement, those not diagnosed with TB disease and started on DOT, and without documented TST or IGRA results from their initial screening, should be evaluated for latent M. tuberculosis infection (LTBI). LTBI evaluated should consist of either a tuberculin skin test (TST) or interferon-gamma release assay (IGRA). Orphans with a negative test for TB infection should have LTBI testing repeated 6 months after arrival.
Receipt of bacille Calmette-Guérin (BCG) vaccine is not a contraindication to a TST, and a positive TST result should not be attributed to BCG vaccine. A patient with a known positive TST should not have the skin test repeated as it may provoke a local reaction. Elements of the medical history for TB should include:
- Previous history of TB
- Illness suggestive of TB (such as cough of >3 weeks duration, dyspnea, weight loss, fever, or hemoptysis)
- Prior treatment suggestive of TB treatment (especially if incomplete of discontinued)
- Prior diagnostic evaluation suggestive of TB
Children are less likely than adults to present with “classic” signs and symptoms of TB such as night sweats, hemoptysis or cavitary findings on chest x-ray. Children more frequently present with generalized findings such as fever, growth delay, and weight loss. Children are also more prone to extra-pulmonary TB, such as meningitis, and disease of the middle ear and mastoid, lymph nodes, bones, joints, and skin. Clinical symptoms can be subtle. The clinician should keep in mind that TB can present with virtually any sign or symptom and should be included in the differential diagnosis of most abnormal clinical findings.
Pertinent elements of the physical exam specific for TB include:
- Thorough pulmonary examination
- Inspection and palpation of appropriate lymph nodes
- Inspection for scars of scrofula, and prior chest surgery
Vaccine Preventable Diseases
Vaccine preventable diseases (VPD) are another important public health consideration for this population. Haiti provides BCG, diphtheria, pertussis (whooping cough) and tetanus (DTwP); measles rubella (MR); oral poliovirus (OPV); and tetanus and diphtheria toxoids (Td), as part of its routine immunization schedule (along with Vitamin A).
However, vaccination coverage rates are low for most of these vaccines. For example in 2008, coverage formeasles vaccination was 58%, third dose DTP 53%, and third dose polio 52%. Moreover, Haiti does not provide a 2nd measles dose, hepatitis A, hepatitis B, Haemophilus influenzae type b (Hib), rubella, varicella, rotavirus, meningococcal, or pneumococcal vaccinations which are considered routine childhood immunizations in the U.S.
In general, when data are available for the orphans in a country, written documentation of immunizations (if available) can be accepted as evidence of adequacy of previous immunization if the vaccines, dates of administration, number of doses, intervals between doses, and age of the child at the time of immunization, are consistent internally and comparable to current US or World Health Organization schedules
However, given the limited data available regarding verification of immunization records in Haitian orphans, and the known low vaccine coverage rates in Haiti, it may be preferred to re-immunize the child presumptively. It is also acceptable to perform a serologic evaluation of concentrations of antibodies to vaccines for certain antigens (i.e. measles, mumps, rubella, hepatitis A, polio, tetanus, and diphtheria) (CDC. General Recommendations on Immunization.)
MMWR 2006;55 (No. RR-15):[34]). Because the rate of more serious local reactions after diphtheria, tetanus, and pertussis (DTaP) vaccine increases with the number of doses administered, serologic testing for antibody to tetanus and diphtheria toxins before re-immunizing (or if a serious reaction occurs) can be considered if appropriate immunization is in question.
Serologic testing for the surface antigen of the hepatitis B virus (HBsAg) should be performed on all children to identify chronic infection. If serologic testing is not available and receipt of immunogenic vaccines cannot be ensured, the prudent course is to provide the immunization series.
We should ensure they are immunized or otherwise immune to hepatitis A virus infection before international travel to pick up the child. If this is not feasible, serologic testing of the orphan for hepatitis A IgM and IgG is recommended, to identify current/recent or past infection. If a child has no evidence of a previous infection, the child should be immunized against hepatitis A according to the recommended immunization schedule. If IgG tests positive, indicating past infection, no immunization will be required for the child. If IgM is positive, indicating current/recent infection, all close contacts and family members should be immunized. Orphans or their household or other close contacts with symptoms consistent with acute viral hepatitis should be evaluated promptly.
HIV
Screening for HIV should be performed on all orphans from Haiti. Transplacentally acquired maternal antibody in the absence of infection can be detected in a child younger than 18 months of age. Hence, positive HIV antibody test results in asymptomatic children of this age require clinical evaluation, further testing (follow-up serologic and PCR), and counseling.
Intestinal Parasites
Since a nationwide survey on intestinal helminths in 5792 urban and rural school children conducted in Haiti in 2002, 34% of stools tested positive for intestinal helminths with the following parasites identified: Ascaris lumbricoides (27.3%), Trichuris trichiura (7.3%), Necator americanus (3.8%), Hymenolepsis nana (2%), Taenia sp. (0.3%) and Strongyloides stercoralis (0.2%) (Champetier de Ribes et al, Bull Soc Pathol Exot. 2005 Jun; 98(2):127-32). Most experts would perform three stools for ova and parasite (O&P) testing collected on three consecutive mornings on all children, regardless of symptoms. If stool O & P examinations are negative and the child has eosinophilia (absolute eosinophil count exceeding 450 cells/mm3), then strongyloides species serologic testing is recommended as stool O&P have poor sensitivity for this infection and the disease can be chronic and lead to serious morbidity (Red Book®: 2009 Report of the Committee on Infectious Diseases – 28th Ed. 2009). If gastrointestinal tract signs or symptoms are present, send stool specimens for culture, and stool antigen testing for giardia, cryptosporidia, and rotavirus.
Malaria
Over 99% of the malaria parasite species that causes malaria in Haiti is P. falciparum, where it is endemic. It has been reported that up to 75% of the population of Haiti lives in malarious areas, especially at altitudes <300 m above sea level (Garcia-Martin, Am J Trop Med Hyg. 1972; 21:617–33). Therefore, it is recommended to screen symptomatic orphans for malaria with a malaria smear. Treatment guidelines can be found on the CDC website
(Guidelines for Treatment of Malaria in the United States).
Syphilis
Clinicians should screen each orphan for syphilis by reliable nontreponemal and treponemal serologic tests. Children with positive treponemal serologic test results should be evaluated by someone with special expertize to assess the differential diagnosis of pinta, yaws, and syphilis and to determine the extent of infection so appropriate treatment can be administered.
Mental Health
Because of stigma in Haitian culture around mental illness, many children may be reluctant to discuss or admit to mental health problems. Likewise, prior caregivers in Haiti may not have fully explored such issues, even prior to the earthquake. The experience of the January 2010 Haitian earthquake would be expected to impact greatly on many of the orphans exposed.
Clinicians should consider potential mental health and developmental issues. When mental health referrals are warranted, added care should be made to explain and arrange such referrals to the patient and his/her caregivers in a culturally sensitive, supportive, and non-stigmatizing way.
Conclusion
This document presents recommendations for an immediate medical screening of Haitian orphans. This is not a comprehensive examination, and it is strongly recommended to have a comprehensive medical history and physical examination once they arrive at their final destination to evaluate other medical and developmental issues in the child, including hearing and vision assessment, valuation of growth and development, blood lead concentration, complete blood cell count with red blood cell indices, newborn screening and/or measurement of thyroid-stimulating hormone concentration, and examination for congenital anomalies (including fetal alcohol syndrome). (Red Book®: 2009 Report of the Committee on Infectious Diseases – 28th Ed. 2009).
The consensus is that no harm would be caused to the kids by overlapping the same Immunization or immunizations. It is a very common place to “catch a child up ” and the CDC has a designated schedule for children with unknown or incomplete records.
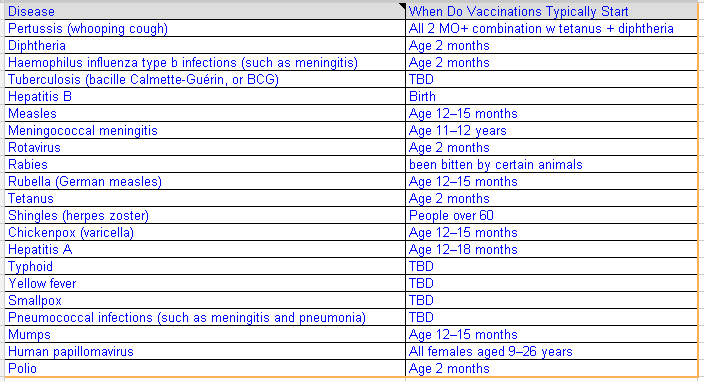
Routine Haiti Immunization Schedule
- BCG Baccile Calmette Guerin vaccine (for TB) at birth
- DTwP Diptheria and tetanus with who cell pertussis vaccine 6, 10, 14 weeks
- MR Measles/ rubella 9mos
- OPV oral polio vaccine, 15 days, 6 wks, 10 wks, 14 wks
- TD Tetanus/ diphtheria toxoid for older children 15yrs +
- Vitamin A supplement 6, 10, 14 18, 30 and 42 mos
MSPP_Recommended-immunization-schedule-for-persons-aged-0-through-6-years—United-States-2012
MSPP_Recommended-immunization-schedule-for-persons-aged-7-through-18-years—United-States-2012
Tableau_des_vaccinations_recommandees_chez_les_enfants_et_adolescents
Tableau_des_vaccinations_recommandees_chez_les_adultes
Lancement-officiel-en-Haïti-du-vaccin-PENTAVALENT
Our goal is to achieve an energy balance and a healthy weight by providing and promoting the following:
- Increase consumption of local fruits and vegetables, legumes, whole grains, and nuts;
- Essential micronutrients such as vitamins and certain minerals.
- Sufficient essential “complete protein” to provide all essential amino acids;
- Examples of foods with protein concentrations greater than 7 percent include soybeans, lentils, kidney beans, white beans, mung beans, chickpeas, cowpeas, lima beans, pigeon peas, lupines, wing beans, almonds, Brazil nuts, cashews, pecans, walnuts, cotton seeds, pumpkin seeds, sesame seeds, spirulina and sunflower seeds.
- Examples of food staples and cereal sources of protein, each with a concentration greater than 7 percent, are (in no particular order) buckwheat, oats, rye, millet, maize (corn), rice, wheat, spaghetti, bulgar, sorghum, amaranth, and quinoa.
- Read more about Diet-Diversity-in-Rural-Haiti.
- High-protein foods include:
| Food | Amount of protein |
|---|---|
| Soy protein isolate | 80 g per 100 g |
| Boiled soybeans | 12 g per 100 g |
| Whey protein concentrate | up to 89 g per 100 g (Average, varies between brands) |
| Whey protein isolate | 90+ g per 100 g (Average, varies between brands) |
| Peanuts* | 24 g per 100 g |
| Hamburger patty | 26 g per 100 g |
| Steak | 27 to 34 g per 100 g |
| Chicken breast* | 31 g per 100 g |
| Tuna fillet | 30 g per 100 g |
| Tuna, canned* | 26 g per 100 g |